Retina Evaluation
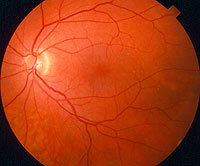 A healthy retina is essential to maintaining clear vision and overall eye functioning. A retinal exam may be recommended by your doctor if any potential retinal abnormalities were detected during a general eye exam, or for patients at a higher risk of developing retinal conditions such as glaucoma, diabetic retinopathy, macular degeneration, retinal detachment and more.
A healthy retina is essential to maintaining clear vision and overall eye functioning. A retinal exam may be recommended by your doctor if any potential retinal abnormalities were detected during a general eye exam, or for patients at a higher risk of developing retinal conditions such as glaucoma, diabetic retinopathy, macular degeneration, retinal detachment and more.
During a retinal exam and consultation, your doctor will perform series of diagnostic procedures in order to evaluate the retina for any signs of disease or abnormalities. These tests may include visual field test, fluorescein angiography, fundus photography and more.
Your doctor will take the time to discuss the results of your exams, as well as any potential risks of retinal disease with you. Patient education and understanding is a top priority of our practice, as it often help patients achieve the most effective treatment as they know how to care for their condition.
Diabetic Retinopathy
Diabetic retinopathy is a complication of diabetes that weakens the blood vessels that supply nourishment to the retina (the light-sensitive lining in the back of the eye where vision is focused). These weak vessels can leak, swell or develop thin branches, causing a loss of vision. Changes to your vision may not be noticeable at first. But in its advanced stages, the disease can cause blurred or cloudy vision, floaters and blind spots – and, eventually, blindness. This damage is irreversible. Diabetic retinopathy is the most common diabetic eye complication and a leading cause of blindness in American adults. Macular edema, which is leaking fluid that causes blurred vision, often occurs with diabetic retinopathy.
Fortunately, diabetic retinopathy is preventable. People with diabetes are most susceptible to developing it, but your risk is reduced if you follow your prescribed diet and medications, exercise regularly, control your blood pressure, and avoid alcohol and cigarettes. Regular eye exams are an integral part of making sure your eyes are healthy. Diabetic retinopathy can be detected through a visual acuity test, a dilated eye exam or tonometry.
Luckily there are some new treatments including laser and intra-ocular injections that can help reverse vision loss in some cases, but prompt and urgent medical evaluation is needed to increase the chance of success. Patients diagnosed with the condition can be treated to slow its progression and prevent further vision loss. Treatment modalities include laser and surgical procedures.
Macular Degeneration Evaluation
 The macula is a part of the retina in the back of the eye that ensures that our central vision is clear and sharp. Age-related macular degeneration (AMD) occurs when the arteries that nourish the retina harden. Deprived of nutrients, the retinal tissues begin to weaken and die, causing vision loss. Patients may experience anything from a blurry, gray or distorted area to a blind spot in the center of vision.
The macula is a part of the retina in the back of the eye that ensures that our central vision is clear and sharp. Age-related macular degeneration (AMD) occurs when the arteries that nourish the retina harden. Deprived of nutrients, the retinal tissues begin to weaken and die, causing vision loss. Patients may experience anything from a blurry, gray or distorted area to a blind spot in the center of vision.
AMD is the number-one cause of vision loss in the U.S. Macular degeneration doesn't cause total blindness because it doesn't affect the peripheral vision. Possible risk factors include genetics, age, diet, smoking and sunlight exposure. Regular eye exams are highly recommended to detect macular degeneration early and prevent permanent vision loss.
Symptoms of macular degeneration include:
- A gradual loss of ability to see objects clearly
- A gradual loss of color vision
- Distorted or blurry vision
- A dark or empty area appearing in the center of vision
There are two kinds of AMD: wet (neovascular/exudative) and dry (non-neovascular). About 10-15% of people with AMD have the wet form. "Neovascular" means "new vessels." Accordingly, wet AMD occurs when new blood vessels grow into the retina as the eye attempts to compensate for the blocked arteries. These new vessels are very fragile, and often leak blood and fluid between the layers of the retina. Not only does this leakage distort vision, but when the blood dries, scar tissue forms on the retina as well. This creates a dark spot in the patient's vision.
Dry AMD is much more common than wet AMD. Patients with this type of macular degeneration do not experience new vessel growth. Instead, symptoms include thinning of the retina, loss of retinal pigment and the formation of small, round particles inside the retina called drusen. Vision loss with dry AMD is slower and often less severe than with wet AMD.
Recent developments in ophthalmology allow doctors to treat many patients with early-stage AMD with the help of lasers and medication.
Retinal Tear & Detachment
The vitreous is a clear liquid that fills our eyes and gives them shape. When we are young, the vitreous has a thick, gelatinous consistency and is firmly attached to the retina. As we age, the vitreous thins and separates from the retina. Although this usually results in nothing more than a few harmless floaters, tension from the detached vitreous can sometimes tear the retina.
If liquid seeps through the tear and collects behind the retina or between its nerve layers, the retinal tear can become a retinal detachment. Retinal detachment can cause significant, permanent vision loss and requires immediate medical treatment.
There are three kinds of retinal detachment. The most common form, described above, occurs when fluid leaks into the retina; people who are nearsighted or who have had an injury or eye surgery are most susceptible. Less frequently, friction between the retina and vitreous or scar tissue pulls the retina loose, something that occurs most often in patients with diabetes. Third, disease-related swelling or bleeding under the retina can push it away from the eye wall.
Signs of retinal tear or detachment include flashes of light, a group or web of floaters, wavy or watery vision, a sense that there is a veil or curtain obstructing peripheral vision, or a sudden drop in vision quality. If you experience any of these symptoms, call your doctor immediately. Early treatment is essential to preserve your vision and is usually done through laser and cryoprobe procedures.
Retinal Vein Occlusion Treatment
A retinal vein occlusion occurs when an artery supplying blood to the eye hardens or swells and presses on a nearby vein and blocks it, making it difficult for blood to leave the eye. The restricted circulation leads to high pressure in the eye, which can in turn cause swelling, bleeding, growth of abnormal blood vessels, and partial or total vision loss.
Vascular occlusions do not cause a change in physical appearance, and they can occur with no pain or noticeable loss of vision. For these reasons, it is important to have routine eye exams and also to check one's own vision by closing one eye at a time.
Luckily there are some new treatments including laser and intra-ocular injections that can help reverse vision loss in some cases, but prompt and urgent medical evaluation is needed to increase the chance of success. It is critical to control high blood pressure, high cholesterol, diabetes and other health conditions that increase the risk of vascular hardening, narrowing and blood clotting.
High Blood Pressure Retinal Evaluation
Patients with high blood pressure (hypertension) are often at a higher risk for developing retinal conditions such as retinal vein occlusions, branch retinal artery occlusions and other conditions that involve damage to the veins and arteries within the eyes. In retinal vein occlusion, veins or arteries in the retina can harden and swell, and may eventually become blocked, or occluded, making it difficult for blood to leave the eye.
There are several different types of retinal vein occlusion, each affecting different veins or arteries within the eye. Aside from high blood pressure, this condition may also be affected by smoking, glaucoma and diabetes, and is most common in patients over the age of 50.
To reduce the risk of developing one or more of these conditions, patients should undergo routine testing so that any signs of vascular damage can be detected as early as possible. Retinal vein occlusions can be detected through a regular retinal exam. Your doctor may also perform a fluorescein angiography in order to confirm the diagnosis of this condition.
Luckily there are some new treatments including laser and intra-ocular injections that can help reverse vision loss in some cases, but prompt and urgent medical evaluation is needed to increase the chance of success. Controlling blood pressure, cholesterol, diabetes and other factors can also help reduce a patient's risk of developing retinal artery damage.
Retinal Complications of Trauma
Eye trauma may occur as a result of an accident, scratch, puncture or contamination, often causing swelling, redness, bleeding, pain and other troubling symptoms for patients of all ages.
Types of Complications Depending on the type and severity of the injury, patients may experience certain retinal complications as a result of trauma to the eye. Retinal tears and detachment may result from blunt injury, which involves the vitreous pulling away from the retina either partially or completely, and allowing fluid to travel between the retina and the vitreous wall. This condition often causes flashes and floaters to develop in the vision, and can cause peripheral vision loss over time.
Retinal hemorrhaging may also occur from trauma, causing bleeding within the retina that occurs within the blood vessels of the retina and can lead to temporary or permanent loss of visual acuity.
Treatment
It is important for patients with retinal tears and other types of ocular injuries to seek immediate treatment for their condition in order to reduce the risk of complications. Treatment for a retinal tear or detachment usually involves laser or cryoprobe treatment to repair the damage and preserve vision.
The best treatment for trauma complications is to prevent the trauma from occurring in the first place. It is important to take the necessary precautions to protect the eyes during sports and other potentially dangerous activities.

